SCAN GAUGE ACCURACY
Why Nexus? Why digital? and what does it mean for the patient?
To better understand the complexities of full-arch prosthetics, first the foundations must be understood, including:
Clinical Acceptability
Implant Position Data
Prosthetic Passivity
Clinical Acceptability
What is considered clinically acceptable, and what matters for complete-arch restorations?
Is there a universally acceptable level of accuracy, misfit, or passivity?
Literature
Some studies have suggested a misfit limit of 10 microns, later increased to 30 microns, and recently proposed an acceptable misfit of up to 150¹ microns. However, to date, there remains no definitive consensus² on the clinically acceptable level of misfit.
Misfits
Misfits in implant superstructures result from cumulative distortions during the final prosthesis fabrication process, often described by the distortion equation.
Clinical
Clinically, a passive fit refers to a case where no long-term clinical issues arise. For screw-retained implant-supported prostheses, this means ensuring there are no static loads or strains within the prosthesis or surrounding bone matrix.
Theoretical
Theoretically, achieving a passive fit hinges on ensuring the summation of distortions equals zero.
Analyzing Implant Data
The fundamental goal of any digital implant scanning technology is to attain accurate and repeatable data. While there are many proposed methods of how to attain implant-location data (Nexus Connect uses a specifically designed process), its important to recognize what methods are used to analyze and review data.
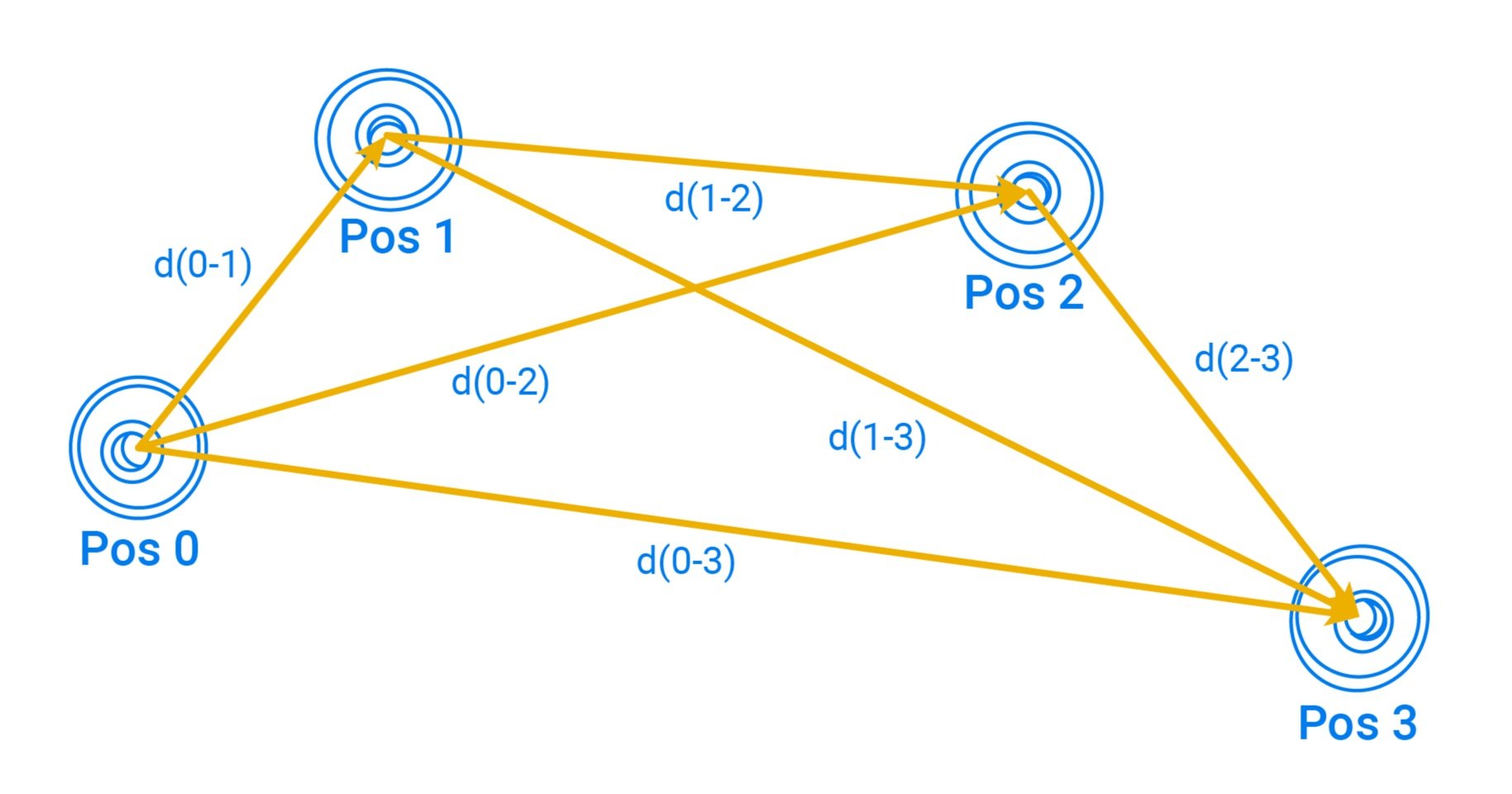
Osteon has applied a method of analyzing implant data using a linear deviation model, comparing a master data set to scanned implant/abutment data.
In 2020 Osteon Medical released the Gen 1.0 Scan Gauge Kit. This design was tested through over 40 iterations before the first version released to the market. To support the engineering theory that was applied when developing the Scan Gauges, a study and internal whitepaper was conducted to determine the accuracy of the data acquisition - Initially in comparison to the only other IOS solutions on the market at the time, conventional scan bodies.
Full Mouth Digital Implant Impressions: A new novel approach. Osteon Medical (2020):
Mean Linear Deviation Analysis
Abstract
The introduction and improvement of intraoral scanning technology has opened the door for the common acquisition of digital dental impressions. However, the accuracy to record multiple implant positions placed on edentulous patients is a common challenge that affects the consistency of the results.
Each intraoral scanner in the market presents a different data acquisition system and different strategies to knit scan data into one file, which causes variations on the scan information. To compensate for this and other sources of error, a special intraoral scan abutment (gauge) and scanning strategy were developed, in order to improve the digital sampling of the arch. In addition, an alignment process was also developed to guarantee that after converting the digital data into numeric values the implant prosthesis can be manufactured achieving an accurate final fit.
Results
9.91 µm: Mean linear deviation of Scan Gauge scans on a 4 implant model.
By contrast, even the best Scanbody group had a mean of 40.17µm. While this is a clear indicator of the Scan Gauge design, it then paved the way for thousands of cases to be completed using this design.
The coordinates from the XML files were compared against the CMM measurement reference. A measurement of linear deviations between each implants of the reference model and each of the XML coordinate implant locations were calculated to conduct the accuracy assessment.
Prosthetic Passivity
Does Digital or Conventional data acquisition methods result in less misfits?
According to a recent study (Shawky et al., 2023): A digital scanner with the aid of an auxiliary device resulted in the best fit in comparison to the conventional and extraoral scanning; Digital approaches resulted in a more accurate fit of a milled PMMA framework with a smaller marginal gap than with conventional impression making.³
Misfit:
Vertical Margin Gap*
50 µm: Intraoral scans with an auxiliary device³
(Using a 3D printed tooth-template with openings for conventional scan bodies, scanning with Primescan IOS)
62 µm: Intraoral scans³
(with conventional scan bodies, scanning with Primescan IOS)
140 µm: Extraoral scanning (of stone cast) using desktop scanner³
*The passivity of fit of the frameworks was tested with the 1-screw test, the terminal screw of the framework assembly was tightened on the multiunit abutment (MUA), and the vertical marginal gap (µm) was measured at the other 3 framework-to-abutment interfaces by using a digital microscope at ×40 magnification.
Among edentulous full arch cases, a digital intraoral scanner along with an auxiliary aid addresses the problem of a lack of anatomic landmarks, thus giving the scanner more spaces with curvature radius changes for its best fit.
Example of milled-titanium framework misfits. Scale and gap is not representative of Shawky et al. study results using PMMA.
What does this mean for prosthetics produced with Nexus Connect Lab?
Nexus Scan Gauges use a variety of design and placement strategies to mitigate the problems with scanning edentulous aches using IOS. In conjunction with the unique scan gauge libraries and scan verification software. These techniques allow the Nexus Scan Gauge system to overcome accuracy and repeatability issues found when using conventional IOS technology or physical impressions. Providing an accurate base point to begin designing a digital full-arch prosthesis.
Utilizing exported abutment data from Nexus Connect is likely to be highly accurate, even when measuring against some of the strictest definitions of clinical acceptability. This is one of the reasons that Nexus Scan Gauge technology has become the pre-eminent full-arch solution in the Australian and United States markets.